Thrombocytopenia (Low Blood Platelets) in Dogs
Some symptoms of ITP
- Bruises on skin, ear flaps, and/or gums
- Bleeding in the sclera (aka “whites of the eyes”) and iris
- Bleeding from nose
- Pale gums
- Acting tired, weakness or collapse
- Shallow, rapid and/or labored breathing
- Bloody urine
- Tar-colored feces or raspberry jam-like feces
- Reduced (or loss of) appetite

By PetPlace
Overview of Thrombocytopenia in Dogs
Thrombocytopenia refers to an abnormally low blood-concentration of platelets, which are blood cells that promote blood clotting after injury to the lining of the blood vessels. When the concentration of platelets becomes too low, bruising and bleeding may occur. Dogs with blood platelet concentrations of less than 40,000 per microliter of blood are at risk for spontaneous bleeding.
Abnormally low platelet numbers in blood can be caused by a variety of disease processes. These include failure to produce new platelets in the bone marrow, premature destruction of circulating platelets often by the body’s own immune system, sequestration or storing of platelets in organs, and consumption of platelets at a rate that exceeds production in the bone marrow.
Dogs of either gender, any age and any breed can suffer from thrombocytopenia.
The severity of bleeding associated with thrombocytopenia depends on how low the platelet numbers fall. In general, the lower the platelet count, the more likely bleeding is to occur.
Overview of Thrombocytopenia in Dogs
Thrombocytopenia refers to an abnormally low blood-concentration of platelets, which are blood cells that promote blood clotting after injury to the lining of the blood vessels. When the concentration of platelets becomes too low, bruising and bleeding may occur. Dogs with blood platelet concentrations of less than 40,000 per microliter of blood are at risk for spontaneous bleeding.
Abnormally low platelet numbers in blood can be caused by a variety of disease processes. These include failure to produce new platelets in the bone marrow, premature destruction of circulating platelets often by the body’s own immune system, sequestration or storing of platelets in organs, and consumption of platelets at a rate that exceeds production in the bone marrow.
Dogs of either gender, any age and any breed can suffer from thrombocytopenia.
The severity of bleeding associated with thrombocytopenia depends on how low the platelet numbers fall. In general, the lower the platelet count, the more likely bleeding is to occur.
Diagnosis of Thrombocytopenia (Low Blood Platelets) in Dogs
Diagnostic tests are needed to recognize thrombocytopenia and exclude other diseases.
Tests may include:
A complete medical history and physical examination. Your veterinarian will ask about previous vaccinations and drug administration as possible factors in the development of thrombocytopenia.
A complete blood count (CBC or hemogram) including a platelet count to identify thrombocytopenia and anemia that may arise from bleeding
Serum biochemistry tests to evaluate for abnormalities in other organ systems and to evaluate the general health
Urinalysis to evaluate for infection, bleeding (hematuria) or protein loss that may occur as a complicating problem in some causes of thrombocytopenia
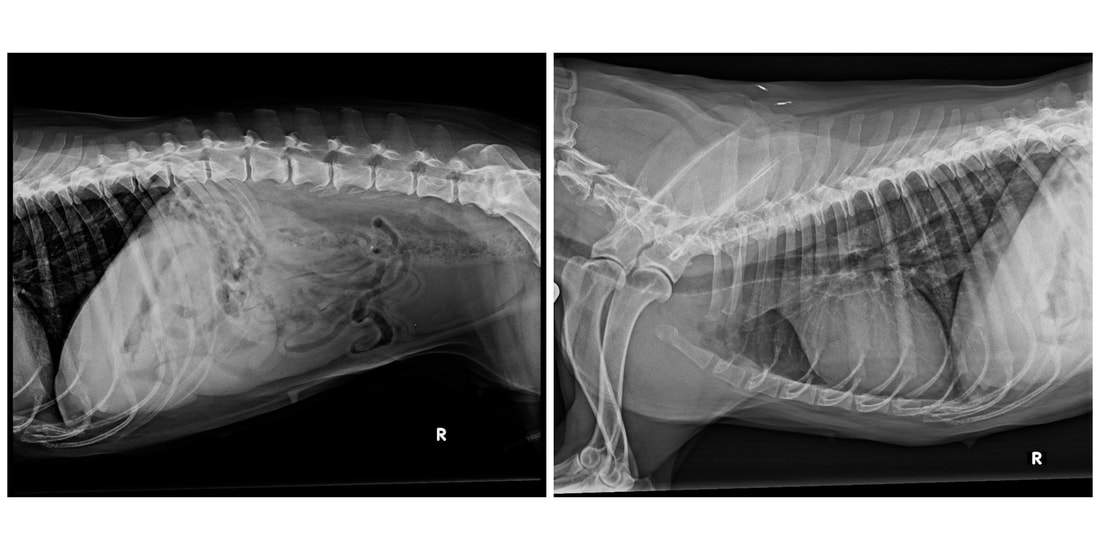
X-rays of the chest or abdomen to evaluate for the presence of other diseases such as infections or cancer that may be associated with thrombocytopenia.
Specific tests for infectious diseases, like tick-borne diseases such as Rocky Mountain Spotted Fever or ehrlichiosis.
Bone marrow aspiration to obtain a sample for laboratory analysis if there is concern that your dog’s bone marrow may not be making adequate numbers of platelets or may have been invaded by cancer. This procedure often is performed under sedation with a local anesthetic to numb the biopsy site.
Other tests of blood clotting. Body-wide abnormalities in coagulation (disseminated intravascular coagulation) can result in massive consumption of platelets.
Immune system function tests if an immune-mediated disease is suspected. In this case the body fails to recognize the platelets as part of itself and attacks them as if they were foreign invaders. The body may consider the platelets as foreign invaders if they become coated with certain drugs or infectious agents.
Diagnostic tests are needed to recognize thrombocytopenia and exclude other diseases.
Tests may include:
A complete medical history and physical examination. Your veterinarian will ask about previous vaccinations and drug administration as possible factors in the development of thrombocytopenia.
A complete blood count (CBC or hemogram) including a platelet count to identify thrombocytopenia and anemia that may arise from bleeding
Serum biochemistry tests to evaluate for abnormalities in other organ systems and to evaluate the general health
Urinalysis to evaluate for infection, bleeding (hematuria) or protein loss that may occur as a complicating problem in some causes of thrombocytopenia
X-rays of the chest or abdomen to evaluate for the presence of other diseases such as infections or cancer that may be associated with thrombocytopenia.
Specific tests for infectious diseases, like tick-borne diseases such as Rocky Mountain Spotted Fever or ehrlichiosis.
Bone marrow aspiration to obtain a sample for laboratory analysis if there is concern that your dog’s bone marrow may not be making adequate numbers of platelets or may have been invaded by cancer. This procedure often is performed under sedation with a local anesthetic to numb the biopsy site.
Other tests of blood clotting. Body-wide abnormalities in coagulation (disseminated intravascular coagulation) can result in massive consumption of platelets.
Immune system function tests if an immune-mediated disease is suspected. In this case the body fails to recognize the platelets as part of itself and attacks them as if they were foreign invaders. The body may consider the platelets as foreign invaders if they become coated with certain drugs or infectious agents.
Treatment of Thrombocytopenia (Low Blood Platelets) in Dogs
Treatment for thrombocytopenia depends on the underlying cause of the low platelet count.
Unless your dog is bleeding, only the underlying cause of the thrombocytopenia is be treated. If a specific cause can be treated successfully, the blood platelet concentration soon returns to normal.
Corticosteroids (cortisone-like drugs) are often used to stop the immune system from destroying platelets.
Antibiotics, especially tetracyclines, often are prescribed until specialized test results for infectious disease are available. Tetracycylines are chosen because
they are effective against bacterial agents called rickettsia that may cause thrombocytopenia, as in ehrlichiosis and Rocky Mountain spotted fever.
It is difficult to increase platelet numbers adequately by transfusion, and transfused platelets do not last very long – a few days at most. Transfusion of whole blood, which contains plasma and all blood cell types including red blood cells and platelets, or packed red cells, which contains red blood cells without plasma, may be necessary in the event of life-threatening hemorrhage or if your dog is anemic from previous blood loss. Platelet-rich plasma is difficult to prepare and is not widely available for dogs.
Treatment for thrombocytopenia depends on the underlying cause of the low platelet count.
Unless your dog is bleeding, only the underlying cause of the thrombocytopenia is be treated. If a specific cause can be treated successfully, the blood platelet concentration soon returns to normal.
Corticosteroids (cortisone-like drugs) are often used to stop the immune system from destroying platelets.
Antibiotics, especially tetracyclines, often are prescribed until specialized test results for infectious disease are available. Tetracycylines are chosen because
they are effective against bacterial agents called rickettsia that may cause thrombocytopenia, as in ehrlichiosis and Rocky Mountain spotted fever.
It is difficult to increase platelet numbers adequately by transfusion, and transfused platelets do not last very long – a few days at most. Transfusion of whole blood, which contains plasma and all blood cell types including red blood cells and platelets, or packed red cells, which contains red blood cells without plasma, may be necessary in the event of life-threatening hemorrhage or if your dog is anemic from previous blood loss. Platelet-rich plasma is difficult to prepare and is not widely available for dogs.
|
Home Care and Prevention
Administer as directed all medications prescribed by your veterinarian. Keep your dog calm and confined indoors to prevent bleeding and bruising. Watch for signs of bleeding or bruising and call your veterinarian immediately if such signs occur or worsen. Prevent tick bites whenever possible because ticks transmit the bacterial agents (rickettsia) that cause ehrlichiosis and Rocky Mountain spotted fever, diseases that cause thrombocytopenia. Use tick preventives and check your dog daily for ticks during warm weather. Other causes of thrombocytopenia are not preventable. |
In-depth Information on Canine Thrombocytopenia
Thrombocytopenia does not always lead to excessive bleeding. Normally, there are more than 600,000 platelets per microliter of blood, which is about one millionth of a quart. Platelet numbers in blood must fall to about 10,000 to 40,000 per microliter before spontaneous bleeding becomes likely. Moderate thrombocytopenia may be found in animals with no evidence of bleeding and this finding often serves as a clue to an important underlying disease process.
Thrombocytopathia is a term that refers to abnormal function of platelets. Animals with thrombocytopathia have adequate numbers of platelets in their blood, but the platelets do not function properly. Thrombocytopathia may be inherited or acquired. Acquired defects in platelet function may be due to drugs (such as aspirin), cancer, or organ failure (such as kidney failure, liver failure).
Coagulation refers to the clotting ability of blood, and normal coagulation arises from the combined effects of properly functioning platelets, blood vessel lining cells (endothelium) and protein clotting factors found in the blood and tissues. Deficiency or abnormal function of any of these components can cause spontaneous bleeding. Occasionally, a disease causes defects in more than one of these components simultaneously.
The following disease processes may cause symptoms similar to those seen in dogs with severe thrombocytopenia:
Vasculitis. This inflammatory disease of blood vessels is characterized by tiny defects in the lining that can allow blood to leak from the vessels. Platelets are attracted to these defects and attempt to plug the holes. Consequently, vasculitis often also results in thrombocytopenia. Several different disease processes can cause vasculitis, including some types of infection and abnormal immune system function that results in an attack against the vessel walls.
Von Willebrand’s disease. The is an inherited defect in a body protein that normally facilitates the attachment of platelets to each other and to damaged vessel walls. Animals with this disorder have prolonged bleeding times and sometimes experience excessive bleeding after minor injury or surgical procedures. It is an inherited trait in several breeds of dogs, notably Doberman pinschers.
Thrombocytopenia does not always lead to excessive bleeding. Normally, there are more than 600,000 platelets per microliter of blood, which is about one millionth of a quart. Platelet numbers in blood must fall to about 10,000 to 40,000 per microliter before spontaneous bleeding becomes likely. Moderate thrombocytopenia may be found in animals with no evidence of bleeding and this finding often serves as a clue to an important underlying disease process.
Thrombocytopathia is a term that refers to abnormal function of platelets. Animals with thrombocytopathia have adequate numbers of platelets in their blood, but the platelets do not function properly. Thrombocytopathia may be inherited or acquired. Acquired defects in platelet function may be due to drugs (such as aspirin), cancer, or organ failure (such as kidney failure, liver failure).
Coagulation refers to the clotting ability of blood, and normal coagulation arises from the combined effects of properly functioning platelets, blood vessel lining cells (endothelium) and protein clotting factors found in the blood and tissues. Deficiency or abnormal function of any of these components can cause spontaneous bleeding. Occasionally, a disease causes defects in more than one of these components simultaneously.
The following disease processes may cause symptoms similar to those seen in dogs with severe thrombocytopenia:
Vasculitis. This inflammatory disease of blood vessels is characterized by tiny defects in the lining that can allow blood to leak from the vessels. Platelets are attracted to these defects and attempt to plug the holes. Consequently, vasculitis often also results in thrombocytopenia. Several different disease processes can cause vasculitis, including some types of infection and abnormal immune system function that results in an attack against the vessel walls.
Von Willebrand’s disease. The is an inherited defect in a body protein that normally facilitates the attachment of platelets to each other and to damaged vessel walls. Animals with this disorder have prolonged bleeding times and sometimes experience excessive bleeding after minor injury or surgical procedures. It is an inherited trait in several breeds of dogs, notably Doberman pinschers.
Insufficient quantities of coagulation proteins. Inherited deficiency of a coagulation protein is known as hemophilia. Certain disease processes such as liver failure can result in acquired deficiency of coagulation proteins.
Warfarin. Ingestion of this compound, a common ingredient in rat poisons, can result in a life-threatening bleeding disorder. Some of the currently available rat poisons contain ingredients that have the same effect as warfarin but are much more potent and longer acting. These poisons affect vitamin K metabolism such that coagulation proteins cannot be properly activated.
Disseminated intravascular coagulation (DIC). This refers to life-threatening bodywide coagulation that occurs as a complication of several serious diseases including infections and cancer. During development of DIC, tiny clots form throughout the body in small blood vessels. Both platelets and coagulation proteins are consumed in the formation of these small clots. Widespread life-threatening bleeding occurs when the body’s platelets and coagulation proteins become depleted.
Disease in specific organs or body locations. Diseases can cause bleeding that is localized to those areas. For example, bladder stones can cause blood in the urine, nasal tumors can cause bleeding from the nostrils (often primarily on one side), gum disease can cause bleeding around the teeth, and trauma can cause bruising or bleeding.
Skin rashes can be mistaken for the tiny pinpoint hemorrhages called petechiae that are found in animals with severe thrombocytopenia. When finger pressure is placed on the red spots in a rash, the redness typically blanches out whereas with petechiae, the redness stays.
In-depth Information on Diagnosis of Canine Thrombocytopenia
Specific diagnostic tests will be needed for your veterinarian to diagnose thrombocytopenia, determine its underlying cause and determine the effects of thrombocytopenia.
Tests may include:
A complete medical history and physical examination. You should be prepared to provide a complete history about your dog. Important questions will be asked about your dog’s home environment including time spent outdoors, travel history, previous illnesses, recent vaccinations, medications (e.g. aspirin, antibiotics) and any symptoms you have noticed. Factors such as your dog’s age, breed and gender will influence the types of diseases your veterinarian will consider as possible causes of thrombocytopenia.
Mild to moderate thrombocytopenia usually does not cause spontaneous bleeding and causes no abnormalities on physical examination. Severe thrombocytopenia, however, often causes characteristic abnormalities on physical examination. These abnormal findings include tiny pinpoint hemorrhages on the gums, whites of the eyes (sclera) or skin called petechiae, and skin bruising called ecchymosis. Bleeding into body cavities or joints is not common in animals with thrombocytopenia. Your veterinarian also may examine the backs of your dog’s eyes (retinas) for evidence of bleeding with an instrument called an ophthalmoscope.
A complete blood count (CBC or hemogram) including a blood platelet concentration to determine if your dog has thrombocytopenia and to evaluate for anemia that may have resulted from blood loss
Serum biochemistry tests to evaluate other organ systems and to determine the general health of your dog
Urinalysis to evaluate for blood in the urine (hematuria), infection, or protein in the urine that may occur with some diseases that cause thrombocytopenia
Unfortunately, a highly reliable diagnostic test is not available for one of the most common causes of severe thrombocytopenia in dogs called immune-mediated thrombocytopenia or idiopathic thrombocytopenic purpura (ITP). Immune-mediated diseases result when the body’s immune system fails to recognize its own cells and tissues and begins to attack them as if they were foreign invaders. In immune-mediated thrombocytopenia, the immune system attacks and destroys platelets. Due to lack of a reliable and specific diagnostic test for this disease, immune-mediated thrombocytopenia usually is diagnosed by ruling out other known causes of thrombocytopenia.
Additional diagnostic tests may be recommended on a case-by-case basis to determine the cause of thrombocytopenia and to insure that your dog receives optimal medical care. Examples of additional tests may include the following:
Tests of the immune system. Systemic lupus erythematosus (SLE) is a generalized autoimmune disease that can cause damage to many tissues such as kidneys, joints, and skin and can result in destruction of platelets. The LE cell preparation and anti-nuclear antibody (ANA) test are two tests that may be requested if your veterinarian suspects your dog may have systemic lupus erythematosus. Immune-mediated destruction of platelets alone is more common than systemic lupus erythematosus.
Tests for specific infectious diseases. Results of the medical history, physical examination and other blood tests often determine whether or not specific tests for infectious diseases are necessary. Some infectious diseases that may be considered include tick-borne diseases such as Rocky Mountain spotted fever and ehrlichiosis. Other infectious diseases can cause blood platelet concentrations to decrease, but most of these other diseases cause only mild thrombocytopenia.
X-rays of the chest or abdomen to evaluate dogs with thrombocytopenia. Enlargement of the spleen often is observed in dogs with immune-mediated thrombocytopenia or infectious causes of thrombocytopenia since the spleen is a common site of platelet destruction. Enlargement of the spleen often can be identified on X-rays of the abdomen.
Abdominal ultrasound examination if your veterinarian suspects a tumor or enlargement of abdominal organs. After clipping the hair and applying a gel to facilitate transmission of ultrasound waves, a probe is held against the abdomen and ultrasound waves create images of the abdominal organs. This same technology is often used in pregnant women to visualize the fetus. If abdominal ultrasound is necessary, your veterinarian may refer your dog to a veterinary radiologist or internist for evaluation.
If a mass or enlarged organ is identified, a biopsy may be recommended to identify the nature of the mass or enlargement. A biopsy specimen may be obtained by surgery or using a specialized biopsy needle inserted through the body wall under ultrasound guidance.
Tests of the immune system. Systemic lupus erythematosus (SLE) is a generalized autoimmune disease that can cause damage to many tissues such as kidneys, joints, and skin and can result in destruction of platelets. The LE cell preparation and anti-nuclear antibody (ANA) test are two tests that may be requested if your veterinarian suspects your dog may have systemic lupus erythematosus. Immune-mediated destruction of platelets alone is more common than systemic lupus erythematosus.
Tests for specific infectious diseases. Results of the medical history, physical examination and other blood tests often determine whether or not specific tests for infectious diseases are necessary. Some infectious diseases that may be considered include tick-borne diseases such as Rocky Mountain spotted fever and ehrlichiosis. Other infectious diseases can cause blood platelet concentrations to decrease, but most of these other diseases cause only mild thrombocytopenia.
X-rays of the chest or abdomen to evaluate dogs with thrombocytopenia. Enlargement of the spleen often is observed in dogs with immune-mediated thrombocytopenia or infectious causes of thrombocytopenia since the spleen is a common site of platelet destruction. Enlargement of the spleen often can be identified on X-rays of the abdomen.
Abdominal ultrasound examination if your veterinarian suspects a tumor or enlargement of abdominal organs. After clipping the hair and applying a gel to facilitate transmission of ultrasound waves, a probe is held against the abdomen and ultrasound waves create images of the abdominal organs. This same technology is often used in pregnant women to visualize the fetus. If abdominal ultrasound is necessary, your veterinarian may refer your dog to a veterinary radiologist or internist for evaluation.
If a mass or enlarged organ is identified, a biopsy may be recommended to identify the nature of the mass or enlargement. A biopsy specimen may be obtained by surgery or using a specialized biopsy needle inserted through the body wall under ultrasound guidance.
If your veterinarian is concerned that your dog’s bone marrow is not producing adequate numbers of platelets, a biopsy or needle aspirate of the bone marrow may be performed. This procedure is performed using a local anesthetic to numb the biopsy site after the animal is sedated.
Other tests of clotting ability may be recommended. Common clotting function tests include prothrombin time and activated partial thromboplastin time, which evaluate two clotting pathways in the body.
In-depth Information on Treatment of Canine Thrombocytopenia
Specific treatment of dogs with thrombocytopenia depends on the cause. If the animal is not bleeding and the platelet count is not seriously low, the underlying cause of the thrombocytopenia is usually treated without specifically attempting to treat the thrombocytopenia itself. If the specific cause of thrombocytopenia can be treated successfully, platelet numbers will increase quickly. The best approach is to treat the underlying disease responsible.
If thrombocytopenia is severe and likely to result in bleeding, the following may be considered:
Blood transfusion. It is difficult to increase the platelet count significantly with blood transfusion alone, and transfused platelets last only hours to days. Despite this, life-threatening bleeding may be treated with transfusion of whole blood, which contains all blood components including plasma and cells; packed red cells, which contain only red blood cells; or platelet-rich plasma, which contains only platelets and plasma.
If your dog is markedly anemic from blood loss, transfusion of whole blood or packed red blood cells may be necessary to provide red cells to carry oxygen to the tissues. Platelet-rich plasma is difficult to prepare and is not widely available in veterinary medicine.
Corticosteroids. Cortisone-like drugs such as prednisone often are used to inhibit destruction of the platelets by the immune system. Immune-mediated destruction of platelets is a common cause of severe thrombocytopenia, and corticosteroids often are used as soon as severe thrombocytopenia is identified.
Antibiotics, tetracyclines. These drugs are often used until results of specific tests for infectious disease are available. Many of the infectious agents that cause thrombocytopenia, such as the rickettsial agents that cause Rocky Mountain Spotted Fever and ehrlichiosis, are responsive to treatment with tetracycline.
Elimination of other drugs. If possible, any drugs your dog was receiving before developing thrombocytopenia will be discontinued because many drugs can cause thrombocytopenia.
Other tests of clotting ability may be recommended. Common clotting function tests include prothrombin time and activated partial thromboplastin time, which evaluate two clotting pathways in the body.
In-depth Information on Treatment of Canine Thrombocytopenia
Specific treatment of dogs with thrombocytopenia depends on the cause. If the animal is not bleeding and the platelet count is not seriously low, the underlying cause of the thrombocytopenia is usually treated without specifically attempting to treat the thrombocytopenia itself. If the specific cause of thrombocytopenia can be treated successfully, platelet numbers will increase quickly. The best approach is to treat the underlying disease responsible.
If thrombocytopenia is severe and likely to result in bleeding, the following may be considered:
Blood transfusion. It is difficult to increase the platelet count significantly with blood transfusion alone, and transfused platelets last only hours to days. Despite this, life-threatening bleeding may be treated with transfusion of whole blood, which contains all blood components including plasma and cells; packed red cells, which contain only red blood cells; or platelet-rich plasma, which contains only platelets and plasma.
If your dog is markedly anemic from blood loss, transfusion of whole blood or packed red blood cells may be necessary to provide red cells to carry oxygen to the tissues. Platelet-rich plasma is difficult to prepare and is not widely available in veterinary medicine.
Corticosteroids. Cortisone-like drugs such as prednisone often are used to inhibit destruction of the platelets by the immune system. Immune-mediated destruction of platelets is a common cause of severe thrombocytopenia, and corticosteroids often are used as soon as severe thrombocytopenia is identified.
Antibiotics, tetracyclines. These drugs are often used until results of specific tests for infectious disease are available. Many of the infectious agents that cause thrombocytopenia, such as the rickettsial agents that cause Rocky Mountain Spotted Fever and ehrlichiosis, are responsive to treatment with tetracycline.
Elimination of other drugs. If possible, any drugs your dog was receiving before developing thrombocytopenia will be discontinued because many drugs can cause thrombocytopenia.
Vincristine. This is a cancer chemotherapy drug that also can accelerate the release of platelets from the bone marrow where they are produced. If the bone marrow is functioning normally, vincristine may be administered to accelerate platelet release from the marrow.
Cyclophosphamide (Cytoxan) and Azathioprine (Imuran) are other drugs that may be used in dogs with suspected immune-mediated thrombocytopenia, especially those dogs that have not responded adequately to corticosteroids. These drugs have strong immunosuppressive effects and also can have potentially serious adverse effects. They should be used only with close veterinary supervision.
Splenectomy. Removal of the spleen may be recommended in dogs with immune-mediated thrombocytopenia that respond poorly to medical treatment. It may also be used in those cases in which sequestration of platelets is suspected, because the spleen is a major site of platelet destruction and sequestration. The spleen is submitted for microscopic examination by a veterinary pathologist after removal. The spleen should not be removed if the thrombocyotpenia is caused by an infectious agent.
Follow-up Care for Dogs with Thrombocytopenia
Optimal treatment for your dog requires a combination of home and professional veterinary care. Follow-up can be crucial. Administer as directed any medications prescribed by your veterinarian and notify your veterinarian if you are experiencing problems treating your dog.
If your dog is at home while his platelet count is very low, keep the animal calm and confined to minimize the chance of bruising and bleeding. Observe your dog closely for signs of bleeding. Look at the whites of the eyes (sclera), gums, and skin for characteristic red spots (petechiae) or bruises (ecchymoses). Call your veterinarian immediately if you observe any petechiae, bruising, or bleeding or if your dog becomes very lethargic or shows any abnormal behavior.
Return to your veterinarian on a regular basis to re-evaluate the platelet count until platelet numbers approach normal. There is no substitute for an accurate blood platelet count.
Cyclophosphamide (Cytoxan) and Azathioprine (Imuran) are other drugs that may be used in dogs with suspected immune-mediated thrombocytopenia, especially those dogs that have not responded adequately to corticosteroids. These drugs have strong immunosuppressive effects and also can have potentially serious adverse effects. They should be used only with close veterinary supervision.
Splenectomy. Removal of the spleen may be recommended in dogs with immune-mediated thrombocytopenia that respond poorly to medical treatment. It may also be used in those cases in which sequestration of platelets is suspected, because the spleen is a major site of platelet destruction and sequestration. The spleen is submitted for microscopic examination by a veterinary pathologist after removal. The spleen should not be removed if the thrombocyotpenia is caused by an infectious agent.
Follow-up Care for Dogs with Thrombocytopenia
Optimal treatment for your dog requires a combination of home and professional veterinary care. Follow-up can be crucial. Administer as directed any medications prescribed by your veterinarian and notify your veterinarian if you are experiencing problems treating your dog.
If your dog is at home while his platelet count is very low, keep the animal calm and confined to minimize the chance of bruising and bleeding. Observe your dog closely for signs of bleeding. Look at the whites of the eyes (sclera), gums, and skin for characteristic red spots (petechiae) or bruises (ecchymoses). Call your veterinarian immediately if you observe any petechiae, bruising, or bleeding or if your dog becomes very lethargic or shows any abnormal behavior.
Return to your veterinarian on a regular basis to re-evaluate the platelet count until platelet numbers approach normal. There is no substitute for an accurate blood platelet count.
Here are two more good articles on explaining this disease
This is my dog's story...

by Holistic And Organix Pet Shoppe
I must start this out with talking about my dog Sydney. She is an American Staffordshire Terrier/Am Bulldog mix. She is 10 yrs old. She has had many medical issues in her past, most all joint related. Hip Dysplasia, CCL tear, unknown cause of bowing out of other knee, Spondylosis and an allergic reaction to Ivermectin (being treated for heartworms) and bee stings. This girl has been around the block more than I can count. I rescued her from a high kill shelter hours before they were to euthanize her. At that time her estimated age was approximately 2 yrs old. She had a scar on her tummy so I assume she had a C-section at some time. I had her spayed after I got her. So a little medical history there before I go further. She has been with me for 8 years now.
In 2015 is when most of her problems began with her joints. Otherwise overall she has been relatively healthy. She has not had vaccines since I got her with exception to the Rabies vaccine and once a Bordetella vaccine by a pushy vet. This past year we decided to titer for the core vaccines and for Rabies instead, due to her poor health with her joints. She overall hasn't had any vaccines in 4 years. Over the last several years she has slowly lost weight. We have no reason at all why at this time. She also has slight hair loss and some pigmentation on her head and tail and some muscle wasting especially in her front legs. Her thyroid is good. No sign of Addison's.
Several weeks ago, her nose began to bleed. She was stressed from storms and it was just a rough day for her overall. The bleeding didn't stop though. This continued off and on for several days. I decided to take her into the vet to get checked out. The vet felt at that time it may have just been a busted blood vessel due to only one nostril bleeding. We had a full work up on blood work including heartworm and pancreas (Spec CPL) to look for more answers. I was planning on having a teeth cleaning and tooth extraction in a week for her, so blood work at her age was important as well. She has a bad tooth that's bothering her. So we came home and things got worse real fast. A few days later, I was back into the vet's office after calling the on-call emergency vet the night before.
I must start this out with talking about my dog Sydney. She is an American Staffordshire Terrier/Am Bulldog mix. She is 10 yrs old. She has had many medical issues in her past, most all joint related. Hip Dysplasia, CCL tear, unknown cause of bowing out of other knee, Spondylosis and an allergic reaction to Ivermectin (being treated for heartworms) and bee stings. This girl has been around the block more than I can count. I rescued her from a high kill shelter hours before they were to euthanize her. At that time her estimated age was approximately 2 yrs old. She had a scar on her tummy so I assume she had a C-section at some time. I had her spayed after I got her. So a little medical history there before I go further. She has been with me for 8 years now.
In 2015 is when most of her problems began with her joints. Otherwise overall she has been relatively healthy. She has not had vaccines since I got her with exception to the Rabies vaccine and once a Bordetella vaccine by a pushy vet. This past year we decided to titer for the core vaccines and for Rabies instead, due to her poor health with her joints. She overall hasn't had any vaccines in 4 years. Over the last several years she has slowly lost weight. We have no reason at all why at this time. She also has slight hair loss and some pigmentation on her head and tail and some muscle wasting especially in her front legs. Her thyroid is good. No sign of Addison's.
Several weeks ago, her nose began to bleed. She was stressed from storms and it was just a rough day for her overall. The bleeding didn't stop though. This continued off and on for several days. I decided to take her into the vet to get checked out. The vet felt at that time it may have just been a busted blood vessel due to only one nostril bleeding. We had a full work up on blood work including heartworm and pancreas (Spec CPL) to look for more answers. I was planning on having a teeth cleaning and tooth extraction in a week for her, so blood work at her age was important as well. She has a bad tooth that's bothering her. So we came home and things got worse real fast. A few days later, I was back into the vet's office after calling the on-call emergency vet the night before.
I had called the clinic earlier to have them go ahead and send over her blood work via email so I could look over them. The blood work showed she had low blood platelets. Her numbers were 12,000. Normal ranges are 175,000-500,000. She was good on her red blood cells so she wasn't anemic although I had noticed her gums turn pale on occasion over the last month or so and some heavy breathing when coming in from outside in 60 degree temps. That usually means heart issues but, her heart was checked and it's fine.
When Sydney took a turn for the worse, she was coughing and gagging on her own blood. It was very scary. She was weak, blood in the iris of her eyes, bruising (gums and belly), no fever, strange stretching, and later discovered she had blood in her urine and her poop.
When Sydney took a turn for the worse, she was coughing and gagging on her own blood. It was very scary. She was weak, blood in the iris of her eyes, bruising (gums and belly), no fever, strange stretching, and later discovered she had blood in her urine and her poop.
I myself had already done a search on her symptoms and it came to the dreaded awful disease called Immune-mediated thrombocytopenia in dogs. It's treated with predisone and chemotherapy drugs. Predisone is usually the first line of defense and if that doesn't work, then chemotherapy drugs are added. What a horrific and scary thought. By the time I got her into the vet, I had not slept for 24 hours straight and my house was a blood bath. I couldn't keep up with the fight. I was exhausted. As soon as my vet saw her blood work, he knew this was serious. He RECHECKED her platelets. In 5 days her platelets bottomed out to ZERO. YES ZERO! This was why she got really sick real fast. Once we returned home from the vet's office, I gave her her first predisone medication. I am so against this drug due to the horrible side effects, so it was VERY hard to give this but due to what was unfolding before my eyes, the exhaustion and Sydney being so miserable, I gave in easily and was ready for anything to just stop this mess so I could get some rest and think this over with a well rested mind as well as how bad Sydney was feeling.
The next day, her poop went from black to brown and her nose was only bleeding a tiny amount. She was very weak. The night before I had taken her into see the vet, she had started this stretching thing. Every time she moved, she stretched..like her muscles were just lacking in water and/or cramping up on her. I still don't have a clue what that was and vet didn't either. After two days on meds, this stopped. She was also weak for several days then she began to get pep back into her step, the nose completely stopped bleeding and she was sleeping normally again. It was a sigh of relief for all of us. The vet wanted us back in 1 week to do a recheck. During this time of recuperating and doing tons of laundry and cleaning walls, doors and floors, I was also still searching. The night before I had ran across a Chinese medicine that's been around for 100's of yrs and many people were using it on their dogs with hemangiosarcoma. I have been researching natural cancer treatments. Upon further reading, discovered it helped the blood to clot faster as well as stopping or slowing internal bleeding of tumors etc. And this is also used in China before people go into have surgery. I found this interesting and was willing to give it a try..after all...with ZERO platelets, what did I have to lose. I'm still reading about this product but so far, not much new that I have found on it. The reviews and comments were very encouraging and if nothing else, helped prolong cancer patients. Now with Sydney we have yet to find cancer. The day we discovered the low platelets, we also did 4 xrays of her torso. No tumors seen on film. If she has one, it's in her nasal cavity or a limb or possibly the bone marrow or blood. But we see no visible swelling or signs of anything so, I assume we have ruled out cancer at this time. If her Spec CPL numbers had of been high, the vet would have suspected pancreatic cancer. So that was ruled out as well along with nothing visible on x-rays.
The next day, her poop went from black to brown and her nose was only bleeding a tiny amount. She was very weak. The night before I had taken her into see the vet, she had started this stretching thing. Every time she moved, she stretched..like her muscles were just lacking in water and/or cramping up on her. I still don't have a clue what that was and vet didn't either. After two days on meds, this stopped. She was also weak for several days then she began to get pep back into her step, the nose completely stopped bleeding and she was sleeping normally again. It was a sigh of relief for all of us. The vet wanted us back in 1 week to do a recheck. During this time of recuperating and doing tons of laundry and cleaning walls, doors and floors, I was also still searching. The night before I had ran across a Chinese medicine that's been around for 100's of yrs and many people were using it on their dogs with hemangiosarcoma. I have been researching natural cancer treatments. Upon further reading, discovered it helped the blood to clot faster as well as stopping or slowing internal bleeding of tumors etc. And this is also used in China before people go into have surgery. I found this interesting and was willing to give it a try..after all...with ZERO platelets, what did I have to lose. I'm still reading about this product but so far, not much new that I have found on it. The reviews and comments were very encouraging and if nothing else, helped prolong cancer patients. Now with Sydney we have yet to find cancer. The day we discovered the low platelets, we also did 4 xrays of her torso. No tumors seen on film. If she has one, it's in her nasal cavity or a limb or possibly the bone marrow or blood. But we see no visible swelling or signs of anything so, I assume we have ruled out cancer at this time. If her Spec CPL numbers had of been high, the vet would have suspected pancreatic cancer. So that was ruled out as well along with nothing visible on x-rays.
One week later we returned for a follow up on blood work (today 2-26-2020). We have been using prednisone, the Chinese herb (Yunnan Baiyao) and I have loaded her up on natural vitamins such as Amla and I have ordered Camu Camu. I have added a little bit of Vitamin D, a good B complex vitamin (as B-12 seems related in these cases as well as vitamin C deficiency) and organic Moringa powder also. She is also getting many probiotics and digestive enzymes. I have removed ginger, fish oils, vitamin E, mushrooms and any anti inflammatory herbs that she was getting. These are considered blood thinners as well as the mushrooms being immune stimulators, something we don't want. I have ordered a hair analysis test kit to check for vitamin and mineral deficiencies to see if anything jumps out. I have also been using Arnica and Phosphorus as she has also some bruising in her front leg that they had tried to get blood from the day of ZERO. The Chinese medicine works for bruising as well. This disease causes bruising and she also had a bruised tummy and gums when she crashed in those couple of days. Her sneezing was crazy in which blood landed everywhere. I am still finding spots of blood. If the homicide detectives ever showed up with a blue light, they would think a massacre happened here.
Moringa is used for “tired blood” (anemia); arthritis and other joint pain (rheumatism); asthma; cancer; constipation; diabetes; diarrhea; epilepsy; stomach pain; stomach and intestinal ulcers; intestinal spasms; headache; heart problems; high blood pressure; kidney stones; fluid retention; thyroid disorders; and bacterial, fungal, viral, and parasitic infections.
Moringa is sometimes applied directly to the skin as a germ-killer or drying agent (astringent). It is also used topically for treating pockets of infection (abscesses), athlete’s foot, dandruff, gum disease (gingivitis), snakebites, warts, and wounds.
The leaves contain 7 times the vitamin C found in oranges, 4 times the calcium in milk, 4 times the vitamin A in carrots, 2 times the protein of yogurt, 25 times the iron in spinach, and 3 times the potassium in bananas.
Various parts of this plant such as the leaves, roots, seed, bark, fruit, flowers and immature pods act as cardiac and circulatory stimulants, possess antitumor, antipyretic, antiepileptic, anti-inflammatory, antiulcer, antispasmodic, diuretic, antihypertensive, cholesterol lowering, antioxidant, antidiabetic, hepatoprotective, antibacterial and antifungal activities.
Moringa is sometimes applied directly to the skin as a germ-killer or drying agent (astringent). It is also used topically for treating pockets of infection (abscesses), athlete’s foot, dandruff, gum disease (gingivitis), snakebites, warts, and wounds.
The leaves contain 7 times the vitamin C found in oranges, 4 times the calcium in milk, 4 times the vitamin A in carrots, 2 times the protein of yogurt, 25 times the iron in spinach, and 3 times the potassium in bananas.
Various parts of this plant such as the leaves, roots, seed, bark, fruit, flowers and immature pods act as cardiac and circulatory stimulants, possess antitumor, antipyretic, antiepileptic, anti-inflammatory, antiulcer, antispasmodic, diuretic, antihypertensive, cholesterol lowering, antioxidant, antidiabetic, hepatoprotective, antibacterial and antifungal activities.
She is on a raw diet and has been for 7 years along with supplements and I made sure I added in some extra liver this past week for added vitamins. I have been reading and researching like a mad woman and just adding in and taking out what may help or do more harm. This disease is idiopathic but has been shown to be caused from vaccines and/or poor diet or tick borne diseases. We did not test for that. We don't have ticks or fleas here so that wasn't even a concern for me. Well she doesn't fit into any of those categories so; this is called Primary or idiopathic ITP with no cause of why it happened.
My vet was hoping to see the platelets up to 50,000 although anything was better than nothing. This was a true test on whether she was responding to the prednisone or not. It was an unsure day of not knowing what the future may hold.
So today, we rechecked the blood and amazingly..her number was 78,000. Not only was the vet amazed and surprised, he felt good about her outcome to tackle this ongoing lifetime disease. So he wants her back in two weeks to retest and see where the platelets are at then. I told him I was hoping for a miracle.
This disease is a lifetime of changes. Sydney will have to be closely monitored her entire life now. Yes this will take some work and adjusting but, in the 8 years I have had her, not once did Sydney ever give up. Now the very first time she went lame with the unknown bowed knee, we didn't do anything for a month. She was so depressed. It was breaking my heart. But then we started going to do hydrotherapy and her attitude changed and you could see hope in her eyes and a determination to get through this. Her depression lifted and off we went for 6 weeks of therapy. To this day, she has been the most determined strong willed dog I have ever known. We don't sit around anymore. We always have a plan. I call her the energizer bunny because she just keeps going. She has gotten through several near death episodes and many debilitating lamenesses and she's still doing ok. Yes I am still hoping to get that tooth out when she becomes stable and I am also hoping to get her hip surgery this summer. Yes some people would say, why would you do that on an old dog. WHY NOT? She isn't dead yet is she? Why should I give up just because she's old. We don't do that with humans, why do it to our pets. After all, they are family.
I told my vet today that very same thing. I have seen it in his eyes along with other vets that feel people should just let go, it isn't worth the fight. Well I beg to differ and I made sure he knew that's how I felt.
The only time I would give up is if she was really really sick and there wasn't anything I could do to help her get better or I have flat out ran out of money. And the very reason I created a fundraiser for her in hopes I don't. If I can find a way, I will help her to the best of my ability. She deserves the best care I can give her, whatever that may be at that time.
My vet was hoping to see the platelets up to 50,000 although anything was better than nothing. This was a true test on whether she was responding to the prednisone or not. It was an unsure day of not knowing what the future may hold.
So today, we rechecked the blood and amazingly..her number was 78,000. Not only was the vet amazed and surprised, he felt good about her outcome to tackle this ongoing lifetime disease. So he wants her back in two weeks to retest and see where the platelets are at then. I told him I was hoping for a miracle.
This disease is a lifetime of changes. Sydney will have to be closely monitored her entire life now. Yes this will take some work and adjusting but, in the 8 years I have had her, not once did Sydney ever give up. Now the very first time she went lame with the unknown bowed knee, we didn't do anything for a month. She was so depressed. It was breaking my heart. But then we started going to do hydrotherapy and her attitude changed and you could see hope in her eyes and a determination to get through this. Her depression lifted and off we went for 6 weeks of therapy. To this day, she has been the most determined strong willed dog I have ever known. We don't sit around anymore. We always have a plan. I call her the energizer bunny because she just keeps going. She has gotten through several near death episodes and many debilitating lamenesses and she's still doing ok. Yes I am still hoping to get that tooth out when she becomes stable and I am also hoping to get her hip surgery this summer. Yes some people would say, why would you do that on an old dog. WHY NOT? She isn't dead yet is she? Why should I give up just because she's old. We don't do that with humans, why do it to our pets. After all, they are family.
I told my vet today that very same thing. I have seen it in his eyes along with other vets that feel people should just let go, it isn't worth the fight. Well I beg to differ and I made sure he knew that's how I felt.
The only time I would give up is if she was really really sick and there wasn't anything I could do to help her get better or I have flat out ran out of money. And the very reason I created a fundraiser for her in hopes I don't. If I can find a way, I will help her to the best of my ability. She deserves the best care I can give her, whatever that may be at that time.
Upon reading many articles, they have claimed this disease can come from multiple sources as to the cause but then many unknown's. Overall, even a single medication can cause this. A vaccine, hepatitis, tick fever, stress, an infection anywhere in the body, and many other reasons. They really don't know what causes it.
As serious as my dog was during the critical period, she was treated with the prednisone and Chinese medicine and nothing else was done. The prednisone worked and I am going to go with my gut that the Chinese herb enhanced that drug to work more sufficiently. My vet knowing my income was limited, made the best decisions and assumptions on what would work..or hopefully would work without costing a fortune. Every single case will vary and when a dog is this critical, you need to know that your vet has your back and will try not to run up costs but in turn save your dog to the best of his ability. My vet has shown his ability to make the right decisions for my dog and in turn, this saved her life at this point because as of now she is comfortable and doing pretty well. We still have a long road to recovery but I know it is all about time, patience and managing the disease. My vet is NOT a holistic vet and does not use natural medicine, but he knows that I do and I let him know about the Chinese meds and what I had read on it so far. I started the Chinese medicine two days after we started the prednisone, so I can't know if both or which is the one working the best. So for now, I say it is both until I discover otherwise. I did also throw in some Arnica and Phosphorus but it only lasted a few days as I had bought the small tubes and used 5 pellets each time. I don't normally use homeopathic medicine but will in times when I feel it could possibly help. One thing about homeopathic, it's safe so I never have to worry.
So for today we are ok. As for the Chinese Herb, it is to be given two ways, 5 days on and 5 days off or give every other day. It can cause high liver markers.
Today is the first day for me not to give it and she seems pretty restless so I may have to switch to every other day. If she is restless the next several days then, that tells me it was working for her when I was giving it. Small changes are noticeable differences in what is and isn't working for her. ~ H.O.P.S.
Stay tuned....
As serious as my dog was during the critical period, she was treated with the prednisone and Chinese medicine and nothing else was done. The prednisone worked and I am going to go with my gut that the Chinese herb enhanced that drug to work more sufficiently. My vet knowing my income was limited, made the best decisions and assumptions on what would work..or hopefully would work without costing a fortune. Every single case will vary and when a dog is this critical, you need to know that your vet has your back and will try not to run up costs but in turn save your dog to the best of his ability. My vet has shown his ability to make the right decisions for my dog and in turn, this saved her life at this point because as of now she is comfortable and doing pretty well. We still have a long road to recovery but I know it is all about time, patience and managing the disease. My vet is NOT a holistic vet and does not use natural medicine, but he knows that I do and I let him know about the Chinese meds and what I had read on it so far. I started the Chinese medicine two days after we started the prednisone, so I can't know if both or which is the one working the best. So for now, I say it is both until I discover otherwise. I did also throw in some Arnica and Phosphorus but it only lasted a few days as I had bought the small tubes and used 5 pellets each time. I don't normally use homeopathic medicine but will in times when I feel it could possibly help. One thing about homeopathic, it's safe so I never have to worry.
So for today we are ok. As for the Chinese Herb, it is to be given two ways, 5 days on and 5 days off or give every other day. It can cause high liver markers.
Today is the first day for me not to give it and she seems pretty restless so I may have to switch to every other day. If she is restless the next several days then, that tells me it was working for her when I was giving it. Small changes are noticeable differences in what is and isn't working for her. ~ H.O.P.S.
Stay tuned....

3-10-2020
Syd goes in Thursday morning for a recheck. Prayers for higher numbers. She had a bad day last Sunday (sleeping almost all day and bruising on inside thigh) but since has done much better. I changed up her TCM (Traditional Chinese Medicine) schedule. Seems to work better for her. Syd has alot going against her and depending on how well she progresses from this disease, will also plan her future. Right now we have alot of unknowns without being able to come up with answers at this time. The best I can do is just help her move forward. I MUST purchase her a small pool for this summer because she has lost alot of muscle mass in her front legs, more on her left side than right. All I can do is help her try to rebuild her muscle. The prednisone she's on will make this worse..so it is imperative I rehab her this summer.
Syd goes in Thursday morning for a recheck. Prayers for higher numbers. She had a bad day last Sunday (sleeping almost all day and bruising on inside thigh) but since has done much better. I changed up her TCM (Traditional Chinese Medicine) schedule. Seems to work better for her. Syd has alot going against her and depending on how well she progresses from this disease, will also plan her future. Right now we have alot of unknowns without being able to come up with answers at this time. The best I can do is just help her move forward. I MUST purchase her a small pool for this summer because she has lost alot of muscle mass in her front legs, more on her left side than right. All I can do is help her try to rebuild her muscle. The prednisone she's on will make this worse..so it is imperative I rehab her this summer.

3-12-2020
I have some FANTASTIC NEWS!! In three weeks Sydney's platelet numbers went from ZERO (day 1), week later 78,000 and now today 2 weeks after that it is up to 342,000. Normal is within 175,000-500,000. He said last time when we were there that he had seen where a lot of dogs with this disease was lucky to get to 150,000. Well we have certainly surpassed that. The vet was very happy and surprised.
I told you I was shooting for a miracle. I strongly feel the use of the Chinese herb along with the meds has made it go up so fast. I think he might be a little more convinced to. He asked what it was I was giving. He said an intern there is experimenting with that. Anyway, now we are reducing dosage to half and gonna hold there for one month on the steroids. He wants her on the steroids for 6 months. We must do this slow so she doesn't have a set back. Sydney has NOT gained any weight at all. She really could stand to gain a couple lbs. He said she may not but she will lose muscle mass. We go back in two weeks for recheck.
I also changed the TCM to every other day as she wasn't doing well with the 5 on 5 off schedule. She's much better on every other day and has much more energy and no more bruising.
I have some FANTASTIC NEWS!! In three weeks Sydney's platelet numbers went from ZERO (day 1), week later 78,000 and now today 2 weeks after that it is up to 342,000. Normal is within 175,000-500,000. He said last time when we were there that he had seen where a lot of dogs with this disease was lucky to get to 150,000. Well we have certainly surpassed that. The vet was very happy and surprised.
I told you I was shooting for a miracle. I strongly feel the use of the Chinese herb along with the meds has made it go up so fast. I think he might be a little more convinced to. He asked what it was I was giving. He said an intern there is experimenting with that. Anyway, now we are reducing dosage to half and gonna hold there for one month on the steroids. He wants her on the steroids for 6 months. We must do this slow so she doesn't have a set back. Sydney has NOT gained any weight at all. She really could stand to gain a couple lbs. He said she may not but she will lose muscle mass. We go back in two weeks for recheck.
I also changed the TCM to every other day as she wasn't doing well with the 5 on 5 off schedule. She's much better on every other day and has much more energy and no more bruising.

4-30-2020
Today we went for a follow up vet visit. WOW we have excellent news for Sydney's ITP. Her numbers have steadily dropped each time we have visited vet (still within normal range though) since the beginning of this in February. Two weeks ago we reduced her prednisone down to half the dose were were giving but yet today..her numbers have gone up. 251,000. Two weeks ago it was 214,000. SO that means her body is making its own platelets. I was shocked and so was my vet. I really didn't expect that but this is great news. Today we go to every other day for the steroids, making this a really low dose. He says we will most likely stay at this dose for awhile. I will also be adding in Vitamin K once a week. It helps with platelets. I ran across this info last night and asked vet about it. He said yes give her some once a week. I did happen to give her some last night. Now the bad news: Due to this disease and the high dose of prednisone that was given, her muscles have wasted away. She can no longer handle walks. We did half a mile walks before this happened and now she cant make it 4 houses down and back. She's really struggling to walk and just overall..get around. I am having to do a lot of lifting and stuff with her. sigh. I have a hurt shoulder too that isn't healing and this is making it worse. This weekend I am putting up a kiddie pool to start therapy on her to try to build her muscles up. Its all we have left to get her muscles back. sigh...alot of work ahead. She is holding her weight at 60 lbs and that's perfect for her right now.
Today we went for a follow up vet visit. WOW we have excellent news for Sydney's ITP. Her numbers have steadily dropped each time we have visited vet (still within normal range though) since the beginning of this in February. Two weeks ago we reduced her prednisone down to half the dose were were giving but yet today..her numbers have gone up. 251,000. Two weeks ago it was 214,000. SO that means her body is making its own platelets. I was shocked and so was my vet. I really didn't expect that but this is great news. Today we go to every other day for the steroids, making this a really low dose. He says we will most likely stay at this dose for awhile. I will also be adding in Vitamin K once a week. It helps with platelets. I ran across this info last night and asked vet about it. He said yes give her some once a week. I did happen to give her some last night. Now the bad news: Due to this disease and the high dose of prednisone that was given, her muscles have wasted away. She can no longer handle walks. We did half a mile walks before this happened and now she cant make it 4 houses down and back. She's really struggling to walk and just overall..get around. I am having to do a lot of lifting and stuff with her. sigh. I have a hurt shoulder too that isn't healing and this is making it worse. This weekend I am putting up a kiddie pool to start therapy on her to try to build her muscles up. Its all we have left to get her muscles back. sigh...alot of work ahead. She is holding her weight at 60 lbs and that's perfect for her right now.

5-15-2020
Well another 'fantastic' news report on Sydney. As you all know that have followed her story, she was diagnosed with ITP (low platelets) back in February. Every 2 weeks we have gone in for rechecks since that first time. Normal numbers range from 165,000-500,000. Her last recheck her numbers were 251,000 which is excellent since she was reduced down to 12.5 mg of prednisone every other day. TODAY her numbers reached 309,000. That is excellent. Also during the last two weeks she's gained another 2 lbs. We need to stop there. She's at 62 lbs now. The vet would have liked her on the meds probably another month but... I am pushing for her to have hip surgery and he wants her off the prednisone completely for 2 weeks prior to surgery. SO, in two weeks we stop the meds completely. Since my vets schedule is full most of the time, we went ahead and scheduled the surgery for June 17th. We will recheck her numbers that morning BEFORE doing surgery to make sure she is ok and won't bleed out. She will also have a rotted tooth removed. Since she is older, we hope her recovery goes well as I will be doing rehabilitation here at home. I will have my hands full and will most likely NOT be available much during the first few days (or week) anyway. Thank you all for being with us throughout this journey.
Well another 'fantastic' news report on Sydney. As you all know that have followed her story, she was diagnosed with ITP (low platelets) back in February. Every 2 weeks we have gone in for rechecks since that first time. Normal numbers range from 165,000-500,000. Her last recheck her numbers were 251,000 which is excellent since she was reduced down to 12.5 mg of prednisone every other day. TODAY her numbers reached 309,000. That is excellent. Also during the last two weeks she's gained another 2 lbs. We need to stop there. She's at 62 lbs now. The vet would have liked her on the meds probably another month but... I am pushing for her to have hip surgery and he wants her off the prednisone completely for 2 weeks prior to surgery. SO, in two weeks we stop the meds completely. Since my vets schedule is full most of the time, we went ahead and scheduled the surgery for June 17th. We will recheck her numbers that morning BEFORE doing surgery to make sure she is ok and won't bleed out. She will also have a rotted tooth removed. Since she is older, we hope her recovery goes well as I will be doing rehabilitation here at home. I will have my hands full and will most likely NOT be available much during the first few days (or week) anyway. Thank you all for being with us throughout this journey.
Sydney passed away in November 2020. She never recovered from the surgery.
Here is her life story....
Here is her life story....