Scroll to bottom for a safe products to use.

By Dr Karen Becker
In parts one and two of this three-part series, Dr. Karen Becker explains the mechanism of Cushing’s disease in pets, the various forms it can take, symptoms to watch for, and how to get a definitive diagnosis of this complex, confusing disorder.
In parts one and two of this three-part series, Dr. Karen Becker explains the mechanism of Cushing’s disease in pets, the various forms it can take, symptoms to watch for, and how to get a definitive diagnosis of this complex, confusing disorder.
Dr. Becker's Comments:
Cushing’s disease was originally diagnosed in a human in 1932 by Dr. Harvey Cushing.
I actually prefer the medical term for the disorder: hyperadrenocorticism. It’s a mouthful, but it’s more descriptive of the condition.
‘Hyper’ means too much, ‘adreno’ refers to the adrenal glands, and ‘corticism’ refers to a syndrome involving the hormone cortisol. Hyperadrenocorticism, loosely translated, means too much cortisol released by the adrenal glands.
Cushing’s disease is rarely seen in kitties. The condition is most often seen in dogs.
Cushing’s disease was originally diagnosed in a human in 1932 by Dr. Harvey Cushing.
I actually prefer the medical term for the disorder: hyperadrenocorticism. It’s a mouthful, but it’s more descriptive of the condition.
‘Hyper’ means too much, ‘adreno’ refers to the adrenal glands, and ‘corticism’ refers to a syndrome involving the hormone cortisol. Hyperadrenocorticism, loosely translated, means too much cortisol released by the adrenal glands.
Cushing’s disease is rarely seen in kitties. The condition is most often seen in dogs.
Cortisol: The Fight-or-Flight Hormone
Cortisol serves a very important function in the body – it is the ‘fight or flight’ hormone. It is designed to be released by the adrenal glands only intermittently and in small amounts, when your dog’s body perceives stress.
When for one reason or another the body up-regulates (turns up) its demand for cortisol, the adrenal glands begin producing the hormone in large amounts, causing toxicity in your pet’s body.
A release of cortisol by the adrenal glands ultimately triggers a glucose release from the liver.
Glucose, which is sugar, provides energy to the cells of the muscles your pet will need to either ‘fight’ or take flight – a dog making a fast escape from a bear, for example -- or a tomcat taking on a new male feline that has invaded his turf.
A release of cortisol doesn’t just trigger a release of glucose and energy to muscles, however.
This powerful hormone impacts a number of important functions in your pet’s body, including:
•Blood pressure
•Electrolyte balance
•Immune function
•Bone and fat metabolism
Cortisol serves a very important function in the body – it is the ‘fight or flight’ hormone. It is designed to be released by the adrenal glands only intermittently and in small amounts, when your dog’s body perceives stress.
When for one reason or another the body up-regulates (turns up) its demand for cortisol, the adrenal glands begin producing the hormone in large amounts, causing toxicity in your pet’s body.
A release of cortisol by the adrenal glands ultimately triggers a glucose release from the liver.
Glucose, which is sugar, provides energy to the cells of the muscles your pet will need to either ‘fight’ or take flight – a dog making a fast escape from a bear, for example -- or a tomcat taking on a new male feline that has invaded his turf.
A release of cortisol doesn’t just trigger a release of glucose and energy to muscles, however.
This powerful hormone impacts a number of important functions in your pet’s body, including:
•Blood pressure
•Electrolyte balance
•Immune function
•Bone and fat metabolism
Too Much of a Good Thing
Your pet needs cortisol in small amounts, but when the adrenal glands over-secrete it, the situation can turn toxic. If your pet experiences symptoms of chronic stress, his adrenal glands will release too much cortisol in response.
It’s important to understand your pet’s body makes no distinction between good and bad stress – it’s all stress. Your dog will have the same physiologic response to an unexpected rabbit in the yard as he will a visit to the groomer. His body interprets the excitement of a trip to the dog park and dealing with a cancerous tumor in the same way.
The Dangers of Excess Cortisol
Chronic stress leads to chronic over-secretion of cortisol, which can result in a multitude of serious health problems, including:
•Elevated blood sugar, which can lead to diabetes
•Elevated blood pressure, which can result in cardiovascular disease
•Extreme hunger from burning all the extra glucose
•Thinning of the skin and coat
•Decreased muscle and bone mass
•Increased risk of infection
Pets that are chronically over-secreting cortisol are considered to be immunosuppressed. They can develop an infection anywhere in their bodies – wherever there is a weak link. Infections of the gums, eyes, ears, skin and the urinary tract are common.
If your dog has recurrent infections or an infection he can’t seem to get rid of, it’s possible too much cortisol is to blame.
Your pet needs cortisol in small amounts, but when the adrenal glands over-secrete it, the situation can turn toxic. If your pet experiences symptoms of chronic stress, his adrenal glands will release too much cortisol in response.
It’s important to understand your pet’s body makes no distinction between good and bad stress – it’s all stress. Your dog will have the same physiologic response to an unexpected rabbit in the yard as he will a visit to the groomer. His body interprets the excitement of a trip to the dog park and dealing with a cancerous tumor in the same way.
The Dangers of Excess Cortisol
Chronic stress leads to chronic over-secretion of cortisol, which can result in a multitude of serious health problems, including:
•Elevated blood sugar, which can lead to diabetes
•Elevated blood pressure, which can result in cardiovascular disease
•Extreme hunger from burning all the extra glucose
•Thinning of the skin and coat
•Decreased muscle and bone mass
•Increased risk of infection
Pets that are chronically over-secreting cortisol are considered to be immunosuppressed. They can develop an infection anywhere in their bodies – wherever there is a weak link. Infections of the gums, eyes, ears, skin and the urinary tract are common.
If your dog has recurrent infections or an infection he can’t seem to get rid of, it’s possible too much cortisol is to blame.
Types of Cushing’s Disease
There are actually several forms of hyperadrenocorticism and it can be confusing to keep them all straight. I’ll do my best to spell it out in an easy-to-understand manner here.
If you have a pet diagnosed with Cushing’s, it’s important for your animal’s health to know exactly what’s going on.
If your pet is healthy, I want to help you keep her that way.
The adrenals are small paired glands covered in fat located in the front of each of your pet’s kidneys.
The adrenal glands are composed of three layers:
1. Zona glomerulosa, the outer, most superficial layer
2. Zona fasciculata, the middle layer
3. Zona reticularis, the deepest layer
The type of Cushing’s your pet acquires depends on which layer of the adrenals is over-secreting hormones.
There are actually several forms of hyperadrenocorticism and it can be confusing to keep them all straight. I’ll do my best to spell it out in an easy-to-understand manner here.
If you have a pet diagnosed with Cushing’s, it’s important for your animal’s health to know exactly what’s going on.
If your pet is healthy, I want to help you keep her that way.
The adrenals are small paired glands covered in fat located in the front of each of your pet’s kidneys.
The adrenal glands are composed of three layers:
1. Zona glomerulosa, the outer, most superficial layer
2. Zona fasciculata, the middle layer
3. Zona reticularis, the deepest layer
The type of Cushing’s your pet acquires depends on which layer of the adrenals is over-secreting hormones.
The middle layer of your pet’s adrenal gland, the zona fasciculata, can over produce glucocorticoids and create what is traditionally known as ‘typical’ Cushing’s disease. Glucocorticoids also go by the name steroids, cortisol, cortisone or prednisone, which is the synthetic version prescribed by veterinarians.
It’s not uncommon for a veterinarian to inadvertently induce typical Cushing’s by prescribing a too-high dose of oral prednisone – or a course of prednisone therapy that is too long in duration. If your pet has taken prednisone, he is predisposed to acquire Cushing’s disease.
While typical Cushing’s involves too much cortisol, ‘atypical’ Cushing’s can occur when the outer layer of the adrenals – the zona glomerulosa – overproduces the hormone aldosterone. Aldosterone balances the electrolytes in your pet’s body.
Atypical Cushing’s disease can also result if the innermost layer, the zona reticularis, begins over producing sex hormones such as estrogen, progesterone or testosterone precursors.
It’s not uncommon for a veterinarian to inadvertently induce typical Cushing’s by prescribing a too-high dose of oral prednisone – or a course of prednisone therapy that is too long in duration. If your pet has taken prednisone, he is predisposed to acquire Cushing’s disease.
While typical Cushing’s involves too much cortisol, ‘atypical’ Cushing’s can occur when the outer layer of the adrenals – the zona glomerulosa – overproduces the hormone aldosterone. Aldosterone balances the electrolytes in your pet’s body.
Atypical Cushing’s disease can also result if the innermost layer, the zona reticularis, begins over producing sex hormones such as estrogen, progesterone or testosterone precursors.
A Closer Look at ‘Typical’ Cushing’s Disease
And as if typical versus atypical hyperadrenocorticism wasn’t confusing enough, the traditional or typical form of the disorder, which involves overproduction of cortisol, also has two types:
1. Adrenal dependent typical Cushing’s
2. Pituitary dependent typical Cushing’s
Hands down, the most common form of Cushing’s disease in pets is the pituitary dependent form.
About 85 percent of dogs with Cushing’s acquire the pituitary dependent form, in which the pituitary gland – the ‘master gland’ in the brain – sends too much stimulating hormone to the adrenals. The adrenal glands respond by over secreting cortisol.
In the remaining 15 percent of adrenal-dependent Cushing’s cases, a tumor develops in an adrenal gland and triggers an up-regulation of cortisol production in the animal’s body.
And as if typical versus atypical hyperadrenocorticism wasn’t confusing enough, the traditional or typical form of the disorder, which involves overproduction of cortisol, also has two types:
1. Adrenal dependent typical Cushing’s
2. Pituitary dependent typical Cushing’s
Hands down, the most common form of Cushing’s disease in pets is the pituitary dependent form.
About 85 percent of dogs with Cushing’s acquire the pituitary dependent form, in which the pituitary gland – the ‘master gland’ in the brain – sends too much stimulating hormone to the adrenals. The adrenal glands respond by over secreting cortisol.
In the remaining 15 percent of adrenal-dependent Cushing’s cases, a tumor develops in an adrenal gland and triggers an up-regulation of cortisol production in the animal’s body.
Which Pets are Most Likely to Acquire Cushing’s Disease?
As I mentioned earlier, it’s very rare for cats to develop Cushing’s.
In the canine population, there are certain breeds genetically predisposed to the disorder including:
•Terriers (silkies, Yorkies, bull terriers and Boston terriers)
•Poodles
•Dachshunds
•American Eskimo dogs/Spitz
Symptoms of Cushing’s Disease
Cortisol is a diverse hormone, which means in excessive amounts it creates a whole host of diverse symptoms.
Most dogs have a few, but not all of the symptoms of the disorder unless diagnosis comes very late in the course of the disease.
The symptoms most commonly seen in dogs with beginning Cushing’s include:
•Increased thirst and urination (which can lead to the symptom of incontinence)
•Increased panting
•Weight gain in the abdominal area, in spite of a reduction in calories
•Thinning skin and change in the pigment of skin, from pink to grey or even black; bruising
•Hair loss
•Irritability or restlessness
As I mentioned earlier, it’s very rare for cats to develop Cushing’s.
In the canine population, there are certain breeds genetically predisposed to the disorder including:
•Terriers (silkies, Yorkies, bull terriers and Boston terriers)
•Poodles
•Dachshunds
•American Eskimo dogs/Spitz
Symptoms of Cushing’s Disease
Cortisol is a diverse hormone, which means in excessive amounts it creates a whole host of diverse symptoms.
Most dogs have a few, but not all of the symptoms of the disorder unless diagnosis comes very late in the course of the disease.
The symptoms most commonly seen in dogs with beginning Cushing’s include:
•Increased thirst and urination (which can lead to the symptom of incontinence)
•Increased panting
•Weight gain in the abdominal area, in spite of a reduction in calories
•Thinning skin and change in the pigment of skin, from pink to grey or even black; bruising
•Hair loss
•Irritability or restlessness
Much less common are symptoms of rear limb weakness and blood clots.
Cushing’s syndrome is so incredibly diverse because every inch of your pet’s body contains cortisol receptors. Because of this, it is often the immunosuppressive aspect of the disease that prompts the first vet visit.
If, for example, your pet has a recurrent urinary tract infection or one that she can’t get rid of, along with one or two other symptoms – perhaps thinning skin or a developing pot bellied appearance, you should ask your veterinarian about Cushing’s disease as a possible cause.
In my practice, most Cushing’s dogs get referred after a misdiagnosed liver disease. The liver of an animal with hyperadrenocorticism gets overtaxed from trying to process the excess cortisol in circulation throughout the body. This causes an elevation in the liver enzyme alanine aminotransferase (ALT) and the inducible liver enzyme, alkaline phosphatase (ALP).
Cushing’s syndrome is so incredibly diverse because every inch of your pet’s body contains cortisol receptors. Because of this, it is often the immunosuppressive aspect of the disease that prompts the first vet visit.
If, for example, your pet has a recurrent urinary tract infection or one that she can’t get rid of, along with one or two other symptoms – perhaps thinning skin or a developing pot bellied appearance, you should ask your veterinarian about Cushing’s disease as a possible cause.
In my practice, most Cushing’s dogs get referred after a misdiagnosed liver disease. The liver of an animal with hyperadrenocorticism gets overtaxed from trying to process the excess cortisol in circulation throughout the body. This causes an elevation in the liver enzyme alanine aminotransferase (ALT) and the inducible liver enzyme, alkaline phosphatase (ALP).
It isn’t uncommon for vets to stop looking once they see the elevated liver enzymes and diagnose liver disease when the problem is actually Cushing’s.
Diagnosing Cushing’s
I recommend you ask for a copy of your dog’s blood test results whenever your vet has them done.
So many dog owners referred to Natural Pet, my hospital, are completely surprised to find out from me that their pet’s liver enzymes have been elevated for two or three years in a row. They want to know why their regular vet didn’t mention it.
Unfortunately, many ‘reactive’ veterinarians just do not address the possibility of Cushing’s until several of the symptoms are present, or a client comes in complaining that a pup is suddenly urinating in the house or losing her hair.
The better, proactive approach is to try to prevent the disease from taking hold. This is why you should get copies of your pet’s blood test results and why every single value that is showing out of the normal range should be investigated.
Your veterinarian should partner with you to identify whether your dog is at risk for pre-Cushing’s symptoms, or is already Cushingoid. If your pet’s ALP value is elevated, ask your vet if this could be the start of Cushing’s disease.
The actual diagnosis of the disease can be difficult. It is typically done through blood tests like the ACTH stimulation test and the low-dose dexamethasone suppression test. Both these tests require at least two blood draws to compare cortisol levels in your dog’s body for a definitive diagnosis of Cushing’s.
I recommend you ask for a copy of your dog’s blood test results whenever your vet has them done.
So many dog owners referred to Natural Pet, my hospital, are completely surprised to find out from me that their pet’s liver enzymes have been elevated for two or three years in a row. They want to know why their regular vet didn’t mention it.
Unfortunately, many ‘reactive’ veterinarians just do not address the possibility of Cushing’s until several of the symptoms are present, or a client comes in complaining that a pup is suddenly urinating in the house or losing her hair.
The better, proactive approach is to try to prevent the disease from taking hold. This is why you should get copies of your pet’s blood test results and why every single value that is showing out of the normal range should be investigated.
Your veterinarian should partner with you to identify whether your dog is at risk for pre-Cushing’s symptoms, or is already Cushingoid. If your pet’s ALP value is elevated, ask your vet if this could be the start of Cushing’s disease.
The actual diagnosis of the disease can be difficult. It is typically done through blood tests like the ACTH stimulation test and the low-dose dexamethasone suppression test. Both these tests require at least two blood draws to compare cortisol levels in your dog’s body for a definitive diagnosis of Cushing’s.
When Cushing’s is confirmed, your vet will want to determine if it’s pituitary or adrenal dependent. In my opinion, the best way to rule out an adrenal gland tumor is with a non-invasive ultrasound test.
Some veterinarians prefer to do a third blood test called a high-dose dexamethasone suppression test to determine whether the source of the cortisol production is adrenal or pituitary dependent.
Whichever method is used, it’s important not only to establish a definitive diagnosis for Cushing’s, but also to determine whether the form of the disease is adrenal or pituitary dependent.
This information will help you and your vet determine the best treatment options available for your sick pet.
An Alternative to More Expensive Diagnostic Testing to Rule Out Cushing’s
If your pet has symptoms of Cushing’s disease but you can’t afford the expensive tests required for a definitive diagnosis, you can ask your veterinarian to do a urine test called the urine cortisol to creatinine ratio test, or the UCC.
The UCC must be run using the first urine of the morning. Results will help your vet determine if your dog is excreting an abnormally high amount of cortisol in his urine.
Circulating levels of cortisol in healthy dogs are quite low, so if there’s a high measurable amount of cortisol in your pup’s urine, it’s a solid clue that Cushing’s may be present and further testing is warranted.
Some veterinarians prefer to do a third blood test called a high-dose dexamethasone suppression test to determine whether the source of the cortisol production is adrenal or pituitary dependent.
Whichever method is used, it’s important not only to establish a definitive diagnosis for Cushing’s, but also to determine whether the form of the disease is adrenal or pituitary dependent.
This information will help you and your vet determine the best treatment options available for your sick pet.
An Alternative to More Expensive Diagnostic Testing to Rule Out Cushing’s
If your pet has symptoms of Cushing’s disease but you can’t afford the expensive tests required for a definitive diagnosis, you can ask your veterinarian to do a urine test called the urine cortisol to creatinine ratio test, or the UCC.
The UCC must be run using the first urine of the morning. Results will help your vet determine if your dog is excreting an abnormally high amount of cortisol in his urine.
Circulating levels of cortisol in healthy dogs are quite low, so if there’s a high measurable amount of cortisol in your pup’s urine, it’s a solid clue that Cushing’s may be present and further testing is warranted.
The UCC is a less expensive way to rule out Cushing’s disease. If your dog’s urine cortisol is within the normal range he most likely does not have typical Cushing’s disease.
Another clue can come from a blood test called the Cortisol Induced Alkaline Phosphate (CiALP) test. Many dogs with adrenal disease have elevated ALP values when bloodwork is done. ALP can be induced (elevated) from a variety of bodily dysfunctions including bone, gallbladder, liver and adrenal disease. This test can determine what percentage of the ALP enzyme level is being caused specifically by the adrenal glands.
The CiALP is a simple and effective screening test to determine whether your pet is starting down the path toward Cushing’s disease. When I have patients with an elevated ALP on routine bloodwork that are also exhibiting any symptoms of Cushing’s disease, I use this simple test to determine if further testing is warranted.
Unfortunately, in the majority of cases, the disease is diagnosed only after full-blown Cushing’s has developed and there’s no holding it back.
Once a dog has full-blown Cushing’s, he will live with the disease for the rest of his life. It’s a horrible illness that can be managed in many cases, but never cured.
Another clue can come from a blood test called the Cortisol Induced Alkaline Phosphate (CiALP) test. Many dogs with adrenal disease have elevated ALP values when bloodwork is done. ALP can be induced (elevated) from a variety of bodily dysfunctions including bone, gallbladder, liver and adrenal disease. This test can determine what percentage of the ALP enzyme level is being caused specifically by the adrenal glands.
The CiALP is a simple and effective screening test to determine whether your pet is starting down the path toward Cushing’s disease. When I have patients with an elevated ALP on routine bloodwork that are also exhibiting any symptoms of Cushing’s disease, I use this simple test to determine if further testing is warranted.
Unfortunately, in the majority of cases, the disease is diagnosed only after full-blown Cushing’s has developed and there’s no holding it back.
Once a dog has full-blown Cushing’s, he will live with the disease for the rest of his life. It’s a horrible illness that can be managed in many cases, but never cured.
Treatment Options
Most of the drugs currently available to treat Cushing’s disease have many undesirable side effects.
It’s extremely important that you discuss your concerns about the possible side effects of any drugs your veterinarian recommends for your pet. Do your own research as well and gauge your own comfort level with giving the medications to your animal.
In my practice, we don’t use most of the Cushing’s drugs because in my opinion, the side effects are usually worse than the symptoms of the disease itself.
In addition to side effects, Cushing’s medications are very expensive and require a great deal of monitoring of bloodwork to ensure the drugs are managed correctly.
Detecting Symptoms Early -- Taking Advantage of the “Gray Zone”
Identifying pre-Cushing’s syndrome as early as possible and reducing your pet’s risk for acquiring the full-blown disease is the approach I recommend.
Dogs don’t suddenly wake up and have Cushing’s disease. The disease happens over time.
Many allopathic vets refuse to acknowledge the beginning of adrenal dysfunction because they don’t know what to do about it until a dog fails the ACTH stimulation (stim) test.
The problem with this approach is it takes months and sometimes years for an animal to be officially labeled with Cushing’s. Waiting this long to take action often means the vet has waited too long.
Most degenerative diseases are not black and white -- non-Cushingoid or Cushingoid. The health of most pets with adrenal symptoms and mild abnormalities on diagnostic tests is somewhere between black and white -- the ‘gray zone.’
Most of the drugs currently available to treat Cushing’s disease have many undesirable side effects.
It’s extremely important that you discuss your concerns about the possible side effects of any drugs your veterinarian recommends for your pet. Do your own research as well and gauge your own comfort level with giving the medications to your animal.
In my practice, we don’t use most of the Cushing’s drugs because in my opinion, the side effects are usually worse than the symptoms of the disease itself.
In addition to side effects, Cushing’s medications are very expensive and require a great deal of monitoring of bloodwork to ensure the drugs are managed correctly.
Detecting Symptoms Early -- Taking Advantage of the “Gray Zone”
Identifying pre-Cushing’s syndrome as early as possible and reducing your pet’s risk for acquiring the full-blown disease is the approach I recommend.
Dogs don’t suddenly wake up and have Cushing’s disease. The disease happens over time.
Many allopathic vets refuse to acknowledge the beginning of adrenal dysfunction because they don’t know what to do about it until a dog fails the ACTH stimulation (stim) test.
The problem with this approach is it takes months and sometimes years for an animal to be officially labeled with Cushing’s. Waiting this long to take action often means the vet has waited too long.
Most degenerative diseases are not black and white -- non-Cushingoid or Cushingoid. The health of most pets with adrenal symptoms and mild abnormalities on diagnostic tests is somewhere between black and white -- the ‘gray zone.’
Dogs headed toward Cushing’s disease, but not yet completely Cushingoid are in the gray zone.
I consider your dog as having pre-Cushing’s syndrome when he exhibits symptoms of Cushing’s disease, but is still able to pass an ACTH stim test. Often there are minor changes in bloodwork; the UCC is borderline or elevated above normal range, and the elevation in ALP has been proven to be cortisol induced.
The majority of allopathic vets will simply wait until a dog becomes Cushingoid, then treat the animal with toxic drugs.
This is never my approach. I am able to reverse many pre-Cushing’s patients with nutraceuticals, Chinese herbs, homeopathics, diet therapy and lifestyle management (reducing biologic stress).
Finding an integrative vet if your pet has Cushing’s symptoms is critical, as this can mean the difference between resolving the problem before it starts, or managing the disease in your pet for the remainder of his life.
Be proactive by having your pet’s ALP level checked annually. Ask your vet to establish a baseline level and address any elevation from the baseline through a screening test like the UCC or CiALP to determine if your dog’s body is over secreting cortisol.
Having this information will help you better manage a pre-Cushing’s situation before it develops to full-blown disease.
Don’t ignore symptoms. If your pup has consistent Cushing’s-type symptoms, no matter how minor, they are absolutely worth investigating for a possible endocrine or adrenal disorder.
Stay tuned for the third and final portion of this three-part series in which I’ll discuss the atypical form of Cushing’s disease, as well as natural treatment and prevention options.
I consider your dog as having pre-Cushing’s syndrome when he exhibits symptoms of Cushing’s disease, but is still able to pass an ACTH stim test. Often there are minor changes in bloodwork; the UCC is borderline or elevated above normal range, and the elevation in ALP has been proven to be cortisol induced.
The majority of allopathic vets will simply wait until a dog becomes Cushingoid, then treat the animal with toxic drugs.
This is never my approach. I am able to reverse many pre-Cushing’s patients with nutraceuticals, Chinese herbs, homeopathics, diet therapy and lifestyle management (reducing biologic stress).
Finding an integrative vet if your pet has Cushing’s symptoms is critical, as this can mean the difference between resolving the problem before it starts, or managing the disease in your pet for the remainder of his life.
Be proactive by having your pet’s ALP level checked annually. Ask your vet to establish a baseline level and address any elevation from the baseline through a screening test like the UCC or CiALP to determine if your dog’s body is over secreting cortisol.
Having this information will help you better manage a pre-Cushing’s situation before it develops to full-blown disease.
Don’t ignore symptoms. If your pup has consistent Cushing’s-type symptoms, no matter how minor, they are absolutely worth investigating for a possible endocrine or adrenal disorder.
Stay tuned for the third and final portion of this three-part series in which I’ll discuss the atypical form of Cushing’s disease, as well as natural treatment and prevention options.
CUSHINGS SYNDROME
By: Dr Dodds DVM
What I have found: imbalances and energetic disturbances in the Pituitary-Adrenal Gland- Pancreas relationships on the physical and electromagnetic levels of the patient.
PHYSICAL LEVEL
MEDICAL DEFINITION: Cushings Syndrome is an endocrine imbalance due to hyperadrenalcorticocism. This means it is caused by an abnormal increased secretion of hormones by the cortex of the Adrenal Gland. These hormones regulate water and electrolytes, blood sugar, sex hormones and natural cortisones. Generally the main defect is in the increased secretion of the glucocorticoid, cortisol.
Hyperfunction of the adrenal cortex can be a result of abnormalities in the cortices, the pituitary or the hypothalamus of the brain. If one sided, the cause can be a tumor in the pituitary (adenomas or adenocarcinomas of the anterior lobe). Or it can be due to a defect in the negative feedback mechanism in the hypothalamus, whereby increasing levels of circulating cortisol (natural cortisone), does not result in physiologic inhibition of the adrenocorticotropic hormone (ACTH) production. In most cases, bilateral adrenocortical hyperplasia is present; adrenocortical tumors are less frequent.
The syndrome can be due to iatrogenics or doctor induced, from administration of therapeutics amounts of corticosteroids (prednisone, prednisilone, depomedrol, etc.) over a protracted period of time. This has been the most frequently found in my EAV studies.
What I have found: imbalances and energetic disturbances in the Pituitary-Adrenal Gland- Pancreas relationships on the physical and electromagnetic levels of the patient.
PHYSICAL LEVEL
MEDICAL DEFINITION: Cushings Syndrome is an endocrine imbalance due to hyperadrenalcorticocism. This means it is caused by an abnormal increased secretion of hormones by the cortex of the Adrenal Gland. These hormones regulate water and electrolytes, blood sugar, sex hormones and natural cortisones. Generally the main defect is in the increased secretion of the glucocorticoid, cortisol.
Hyperfunction of the adrenal cortex can be a result of abnormalities in the cortices, the pituitary or the hypothalamus of the brain. If one sided, the cause can be a tumor in the pituitary (adenomas or adenocarcinomas of the anterior lobe). Or it can be due to a defect in the negative feedback mechanism in the hypothalamus, whereby increasing levels of circulating cortisol (natural cortisone), does not result in physiologic inhibition of the adrenocorticotropic hormone (ACTH) production. In most cases, bilateral adrenocortical hyperplasia is present; adrenocortical tumors are less frequent.
The syndrome can be due to iatrogenics or doctor induced, from administration of therapeutics amounts of corticosteroids (prednisone, prednisilone, depomedrol, etc.) over a protracted period of time. This has been the most frequently found in my EAV studies.
Clinical findings: bilateral symmetrical hairlessness over the back and abdomen. The remaining hair is dry, rough and can be easily pulled out. There is increased thirst and urination, abdomen becomes bloated and as disease progresses, much muscular weakness. Fasting blood glucose levels are higher than normal, with many cases exhibiting overt Diabetes Mellitus. Increased serum potassium levels are associated with generalized muscular weakness. If there are excessive sex hormones produced, an enlarged clitoris may be present in the female dog. Osteoporosis is sometimes seen.
Definitive diagnosis is determined with hormonal blood tests. Differential diagnosis of adrenocortical hyperplasia and neoplasia is often possible by using ACTH stimulation tests. IM injections of 20 units of ACTH gel will cause at least a doubling of the urinary steroids in patients with adrenocortical hyperplasia. Tumors are unresponsive to exogenous ACTH administered.
Orthodox Treatment: depends on the type of lesion present. Localized adrenal cortical tumors are removed surgically with resultant hypofunction of the rest of the adrenal cortex thus necessitating life-long administration of hormone replacement therapy. Pituitary tumor surgery is difficult and is not amenable to routine veterinary practice.
Definitive diagnosis is determined with hormonal blood tests. Differential diagnosis of adrenocortical hyperplasia and neoplasia is often possible by using ACTH stimulation tests. IM injections of 20 units of ACTH gel will cause at least a doubling of the urinary steroids in patients with adrenocortical hyperplasia. Tumors are unresponsive to exogenous ACTH administered.
Orthodox Treatment: depends on the type of lesion present. Localized adrenal cortical tumors are removed surgically with resultant hypofunction of the rest of the adrenal cortex thus necessitating life-long administration of hormone replacement therapy. Pituitary tumor surgery is difficult and is not amenable to routine veterinary practice.
My experience with Cushings I can honestly say is limited, but those cases I have examined with EAV have shown abnormally high energy values in the Adrenal Glands, Pituitary, Liver, Small Intestine, and Colon and lower than normal values in the Pancreas, bone marrow and immune system. Many of these were false Cushings or Iotregenic. I have found these to be reversed by the three D’S:
DIET - Chemical toxins polluting our food and water and increased demands of insulin by heavy concentrations of carbohydrates in commercial diets. Changing the diet from commercial products to home made fresh diet is mandatory.
DETOXIFICATION-EAV analysis of these cases show toxin depositions of the steroid drugs given in the past, vaccinations, heavy metals, pesticides, herbicides, food preservatives, analine dyes, some antibiotics, flea, tick and heartworm drug preventatives.This has required sequential detoxification with specific nosode homeopathics made of these products.
DIET - Chemical toxins polluting our food and water and increased demands of insulin by heavy concentrations of carbohydrates in commercial diets. Changing the diet from commercial products to home made fresh diet is mandatory.
DETOXIFICATION-EAV analysis of these cases show toxin depositions of the steroid drugs given in the past, vaccinations, heavy metals, pesticides, herbicides, food preservatives, analine dyes, some antibiotics, flea, tick and heartworm drug preventatives.This has required sequential detoxification with specific nosode homeopathics made of these products.
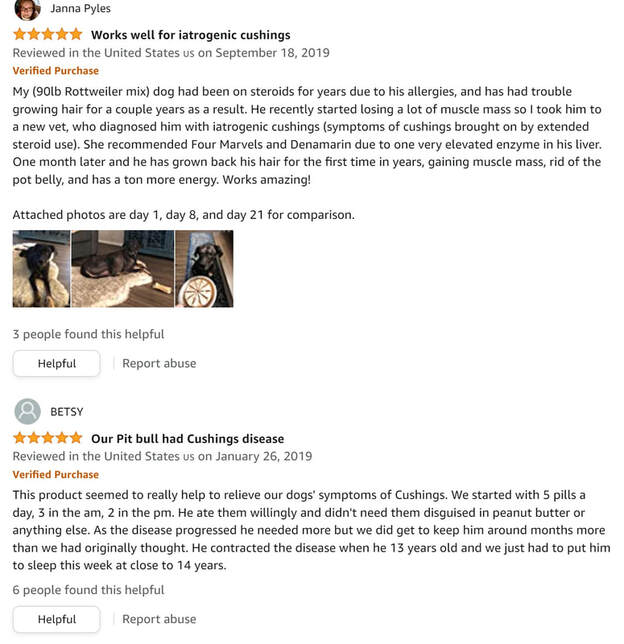
FIGUEROLA Revertol Canine
Revertol is a state-of-the-art nutritional dietary supplement developed to enhance the canine or feline body's ability to naturally address and target Cushing’s syndrome and many of the adverse effects when facing Cushing's. Revertol helps correct hormonal malfunctions and enhance cortisol regulation, and boosts cat's and dog's overall immune system to fight disease and infection.
Cortidopatrophin™:
- Supports the normal functioning of the pituitary gland
- Acts as an anti-inflammatory by supporting the body's ability to inhibit the enzymes that promote inflammation
- Facilitates the uptake of glucose into the cells
- Boosts the immune system, augmenting anti-viral, anti-bacterial, and anti-fungus properties
Directions
Administer 1 capsule twice daily per 30 lbs of body weight.
Ingredients
Cortidopatrophin™ Proprietary Formula: Suppresol™ (D-Glucaric acid, Indole-3-Carbinol), L-Carnosine, Phosphatidylserine, Angi casti fructus (Vitex agnus-castus), Alpha-calacorene, Bis-glycinato oxovanadium (BGOV), Alpha-copaene, Brevifolin, Dehydroepiandrosterone (DHEA), Superoxide Dismutase (SOD), Punica granatum, Carboxylic acids, Withania somnifera, Commiphora mukul, Corilagin, Cymene, Ellagic acid, Ellagitannins, Gallocatechins, Glycyrrhiza glabra extract, Geraniin, Hypophyllanthin, alpha-Pinene, alpha-Thujone, beta-Caryophyllene, beta-Elemene, beta-Pinene, Betaine, Bincatriol, Borneol, Calamenene, Quercetol, Quercetin, Rutin, Camphene, catechins, Cedrucine, Crolechinic acid, Cuparophenol, Gymnemic acid, D-Limonene, Daucosterol, Dihydrobenzofuran, Pterocarpus marsupium extract, Purpurex™ (Purple Corn Extract), Eugenol, Dimethyl cedrusine, Dipentene, Euparophenol, Gallocatechol, gamma-Terpinene, gamma-Terpineol, Hardwickiic acid, Isoboldine, Korberin A, Korberin B, Lignin, Linalool, Magnoflorine, Methylthymol, Myrcene, Norisoboldine, P-Cymene, Tannin, Taspine, Proanthocyanidins, Vanillin, Saponin, Triacontanol, Terpinen-4-ol, Evodiamine extract, Inhibitol® (50% Salicin Complex (Purpura salix, Fillipendula ulmaria and Gaultheria procumbens), 65% Boswellic Acid Extract (Rhizome), 95% Curcuminoids Extract (from Turmeric Extract), 40% Gingerols Extract, 45% Poliphenols (Camelia sinensis), 6% Berberine (Barberry and Chinese goldthread), Alkaloid Complex Extract (Uncaria Tomentosa), Origanum vulgare extract, 2% Ursalic acid (Ocimun basilicum), 95% Procyanidins (Vitis vinifera), 23% Phenolics (Rosmarinus ocinalis), Gamma-Tocopherol (Elais gueneensis), Gamma-Tocotrienol (Elaeis gueneensis), Superoxide Dismutase), Salisorosides, Glycyrrhizic acid, L-Ornithine-Alpha-Ketoglutarate, L-Arginine-Alpha-Ketoglutarate, L-Theanine, Alpha-lipoic acid, Acetyl-L-Carnitine, Phyllanthus niruri extract, Lutein, Zeaxanthin, L-DOPA, Corosolic Acid, L-Tyrosine, Lepidium meyenii, Iodine Forte™ (Kelp extract, Fucoidan, Bladderwrack, Seaweed extract and Red marine algae extract), Spirulina, Vaccinium macrocarpa extract, Trigonella foenumgraecum extract, Omega-Fortis™ (Omega-3 fatty acid, Omega-6 fatty acid and Omega-9 fatty acid), Magnesium oxide 4g, Magnesium chelate 2g, Boron 20mg, Biotin 3mg, Riboflavin 0.4g, Niacinamide 0.5g, Adenine 50mg, Pantothenic Acid 6mg, Pyridoxine 1g, Folic Acid 8mg, Methylcobalamin 50mg, Chromium Polynicotinate 2mg.
Cortidopatrophin™:
- Supports the normal functioning of the pituitary gland
- Acts as an anti-inflammatory by supporting the body's ability to inhibit the enzymes that promote inflammation
- Facilitates the uptake of glucose into the cells
- Boosts the immune system, augmenting anti-viral, anti-bacterial, and anti-fungus properties
Directions
Administer 1 capsule twice daily per 30 lbs of body weight.
Ingredients
Cortidopatrophin™ Proprietary Formula: Suppresol™ (D-Glucaric acid, Indole-3-Carbinol), L-Carnosine, Phosphatidylserine, Angi casti fructus (Vitex agnus-castus), Alpha-calacorene, Bis-glycinato oxovanadium (BGOV), Alpha-copaene, Brevifolin, Dehydroepiandrosterone (DHEA), Superoxide Dismutase (SOD), Punica granatum, Carboxylic acids, Withania somnifera, Commiphora mukul, Corilagin, Cymene, Ellagic acid, Ellagitannins, Gallocatechins, Glycyrrhiza glabra extract, Geraniin, Hypophyllanthin, alpha-Pinene, alpha-Thujone, beta-Caryophyllene, beta-Elemene, beta-Pinene, Betaine, Bincatriol, Borneol, Calamenene, Quercetol, Quercetin, Rutin, Camphene, catechins, Cedrucine, Crolechinic acid, Cuparophenol, Gymnemic acid, D-Limonene, Daucosterol, Dihydrobenzofuran, Pterocarpus marsupium extract, Purpurex™ (Purple Corn Extract), Eugenol, Dimethyl cedrusine, Dipentene, Euparophenol, Gallocatechol, gamma-Terpinene, gamma-Terpineol, Hardwickiic acid, Isoboldine, Korberin A, Korberin B, Lignin, Linalool, Magnoflorine, Methylthymol, Myrcene, Norisoboldine, P-Cymene, Tannin, Taspine, Proanthocyanidins, Vanillin, Saponin, Triacontanol, Terpinen-4-ol, Evodiamine extract, Inhibitol® (50% Salicin Complex (Purpura salix, Fillipendula ulmaria and Gaultheria procumbens), 65% Boswellic Acid Extract (Rhizome), 95% Curcuminoids Extract (from Turmeric Extract), 40% Gingerols Extract, 45% Poliphenols (Camelia sinensis), 6% Berberine (Barberry and Chinese goldthread), Alkaloid Complex Extract (Uncaria Tomentosa), Origanum vulgare extract, 2% Ursalic acid (Ocimun basilicum), 95% Procyanidins (Vitis vinifera), 23% Phenolics (Rosmarinus ocinalis), Gamma-Tocopherol (Elais gueneensis), Gamma-Tocotrienol (Elaeis gueneensis), Superoxide Dismutase), Salisorosides, Glycyrrhizic acid, L-Ornithine-Alpha-Ketoglutarate, L-Arginine-Alpha-Ketoglutarate, L-Theanine, Alpha-lipoic acid, Acetyl-L-Carnitine, Phyllanthus niruri extract, Lutein, Zeaxanthin, L-DOPA, Corosolic Acid, L-Tyrosine, Lepidium meyenii, Iodine Forte™ (Kelp extract, Fucoidan, Bladderwrack, Seaweed extract and Red marine algae extract), Spirulina, Vaccinium macrocarpa extract, Trigonella foenumgraecum extract, Omega-Fortis™ (Omega-3 fatty acid, Omega-6 fatty acid and Omega-9 fatty acid), Magnesium oxide 4g, Magnesium chelate 2g, Boron 20mg, Biotin 3mg, Riboflavin 0.4g, Niacinamide 0.5g, Adenine 50mg, Pantothenic Acid 6mg, Pyridoxine 1g, Folic Acid 8mg, Methylcobalamin 50mg, Chromium Polynicotinate 2mg.
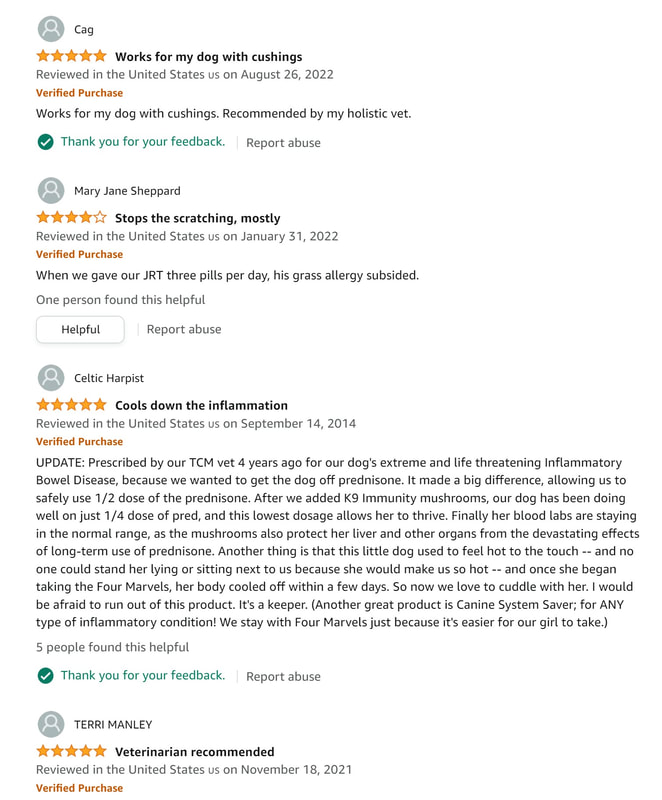
Si Miao San (Four Marvels Powder)
Fantastic product for my dog with colitis.
HMR Lignans
Specially Formulated for Medium Sized Dogs - Bottle contains 90 capsules with 20mg HMR Lignans. Perfect for medium-sized dog breeds! Give one 20mg capsule of HMR lignans orally per every 20lbs of body weight daily up to 4 capsules. Can be administered whole, or capsule can be opened and mixed in with dog's food.
Derived From Norway Spruce Trees - HMR lignan is extracted from the knots of the Norwegian Spruce tree yielding high amounts of Hydroxymatairesinol (HMR) lignans. HMR lignans are phytonutrients with antioxidant, anti-inflammatory, and other properties that may benefit your dog’s health.
Natural Immune System Booster - HMR lignans for dogs added to your pets’ diet may help boost their immune system. Many vets and Universities recommend lignans for dogs as a natural immune system booster as lignans have powerful antioxidant effects that counter oxidative (free radical) damage.
HMR Lignans Holistic Health Benefits - Lignans for dogs support overall health with natural phytonutrients, including; support for cardiovascular function, normal digestion, and sleep patterns. HMR lignans may support skin and coat health, reproductive organ health and promote healthy cortisol levels. Excellent option for dogs with low tolerance to fiber.
Derived From Norway Spruce Trees - HMR lignan is extracted from the knots of the Norwegian Spruce tree yielding high amounts of Hydroxymatairesinol (HMR) lignans. HMR lignans are phytonutrients with antioxidant, anti-inflammatory, and other properties that may benefit your dog’s health.
Natural Immune System Booster - HMR lignans for dogs added to your pets’ diet may help boost their immune system. Many vets and Universities recommend lignans for dogs as a natural immune system booster as lignans have powerful antioxidant effects that counter oxidative (free radical) damage.
HMR Lignans Holistic Health Benefits - Lignans for dogs support overall health with natural phytonutrients, including; support for cardiovascular function, normal digestion, and sleep patterns. HMR lignans may support skin and coat health, reproductive organ health and promote healthy cortisol levels. Excellent option for dogs with low tolerance to fiber.
Melatonin
Melatonin also helps Cushing's disease by inhibiting certain enzymes. A general guideline for dosing melatonin is:
Dogs under 10 lbs – 1 mg of melatonin every 12 hours (also for those who want to give their dogs very low doses of melatonin) (open capsule and pour into foods for breaking down the mg)
10-30 lbs – 3 mg of melatonin 1-2 times a day
30-50 lbs - 3 mg of melatonin 2 times a day
50+ lbs - 3 mg of melatonin 2-3 times a day
Giant dogs or as directed by holistic vet.
20mg capsules here
Dogs under 10 lbs – 1 mg of melatonin every 12 hours (also for those who want to give their dogs very low doses of melatonin) (open capsule and pour into foods for breaking down the mg)
10-30 lbs – 3 mg of melatonin 1-2 times a day
30-50 lbs - 3 mg of melatonin 2 times a day
50+ lbs - 3 mg of melatonin 2-3 times a day
Giant dogs or as directed by holistic vet.
20mg capsules here
Four Marvels (Same as Si Miao San posted above in powder form)
Ingredients
Ingredients: Serving Size: 1 Tablet (500mg) Servings Per Container: 120 Amount Per Serving / % DV Proprietary Blend† 500mg Cang-zhu atractylodes rhizome‚ achyranthes root‚ job's tears seed‚ phellodendron bark. †Daily Value not established. Other Ingredients: Silicon dioxide (glidant/dehydrant)‚ stearic acid (lubricant/binder)‚ microcellulose (coating).
Directions
2-3 times daily.
1-10 lbs: ¼ tablet
11-20 lbs: ½ tablet
21-35 lbs: 1 tablet
36-75 lbs: 2 tablets
76-100 lbs: 3 tablets
If you cant get the tablet in them, these will easily crush up in a tablet crusher.
Ingredients: Serving Size: 1 Tablet (500mg) Servings Per Container: 120 Amount Per Serving / % DV Proprietary Blend† 500mg Cang-zhu atractylodes rhizome‚ achyranthes root‚ job's tears seed‚ phellodendron bark. †Daily Value not established. Other Ingredients: Silicon dioxide (glidant/dehydrant)‚ stearic acid (lubricant/binder)‚ microcellulose (coating).
Directions
2-3 times daily.
1-10 lbs: ¼ tablet
11-20 lbs: ½ tablet
21-35 lbs: 1 tablet
36-75 lbs: 2 tablets
76-100 lbs: 3 tablets
If you cant get the tablet in them, these will easily crush up in a tablet crusher.
A treatment plan specific from NHV
Make sure you add Milk Thistle and SAM-e for the liver. Also for the liver are chinese herbs mixes (Liver Support) and TUDCA.
About TUDCA (Tauroursodeoxycholic Acid):
Bile Salt for Liver Health: TUDCA is considered a liver support supplement since it supports healthy levels of liver enzymes.
Most Powerful Bile Salt for Liver and Gallbladder health: Studies show TUDCA may help optimize the content of gallbladder bile.
Other Health Benefits:
TUDCA is most known for liver health but also supports intestinal, immune, gallbladder, and thyroid health.
About TUDCA (Tauroursodeoxycholic Acid):
Bile Salt for Liver Health: TUDCA is considered a liver support supplement since it supports healthy levels of liver enzymes.
Most Powerful Bile Salt for Liver and Gallbladder health: Studies show TUDCA may help optimize the content of gallbladder bile.
Other Health Benefits:
TUDCA is most known for liver health but also supports intestinal, immune, gallbladder, and thyroid health.